What to do when it all becomes “too much.”
By Shannon Bussnick, LSW

Normalize taking a break
before your cup overflows
If you have Borderline Personality Disorder (BPD) you might notice that the world sometimes feels overwhelming. Or maybe it always feels that way for you. Many people with BPD are not only emotionally sensitive, but also physically sensitive to their environment. Loud noises, bright lights, scratchy fabrics, crowded rooms, an unwelcomed shoulder nudge – these can all crank up stress levels.
In fact, research suggests that BPD’s hallmark emotional intensity often goes hand-in-hand with being easily overwhelmed by sensory input. This heightened sensitivity can make everyday situations feel like a barrage on your senses, often triggering emotional meltdowns when it all becomes ‘too much.’
Disclaimer: The content on this blog is for informational purposes only and is not medical advice. I am not a licensed medical professional. Always consult your healthcare provider before making any changes to your mental health treatment or using mind-altering substances.
If you are in crisis or having thoughts of harming yourself or others, contact emergency services or a mental health professional immediately. Your safety matters.
Sensory Sensitivity and BPD: Understanding the Overlap
Being hyper-vigilant is a common experience in BPD, meaning your brain is constantly scanning for threats – and that doesn’t only apply to emotions or relationships. It can also mean you’re on high alert for physical sensations around you. Many people with BPD report that they get sensory overstimulation alongside their emotional oversensitivity.
In other words, this means your nervous system might turn up the volume on stimuli that other people find easy to tune out. Ever felt attacked by an invisible force just because the room is too noisy, or the lights are flickering? It’s as if there’s no escaping the monster crouched around every corner. Sensory overload can feel like that – your heart might pound, you get sweaty, maybe even feel unreal or disconnected (dissociation can also be common) because your brain is so overwhelmed. It’s not in your head or an overreaction; it’s a genuine physiological stress response.
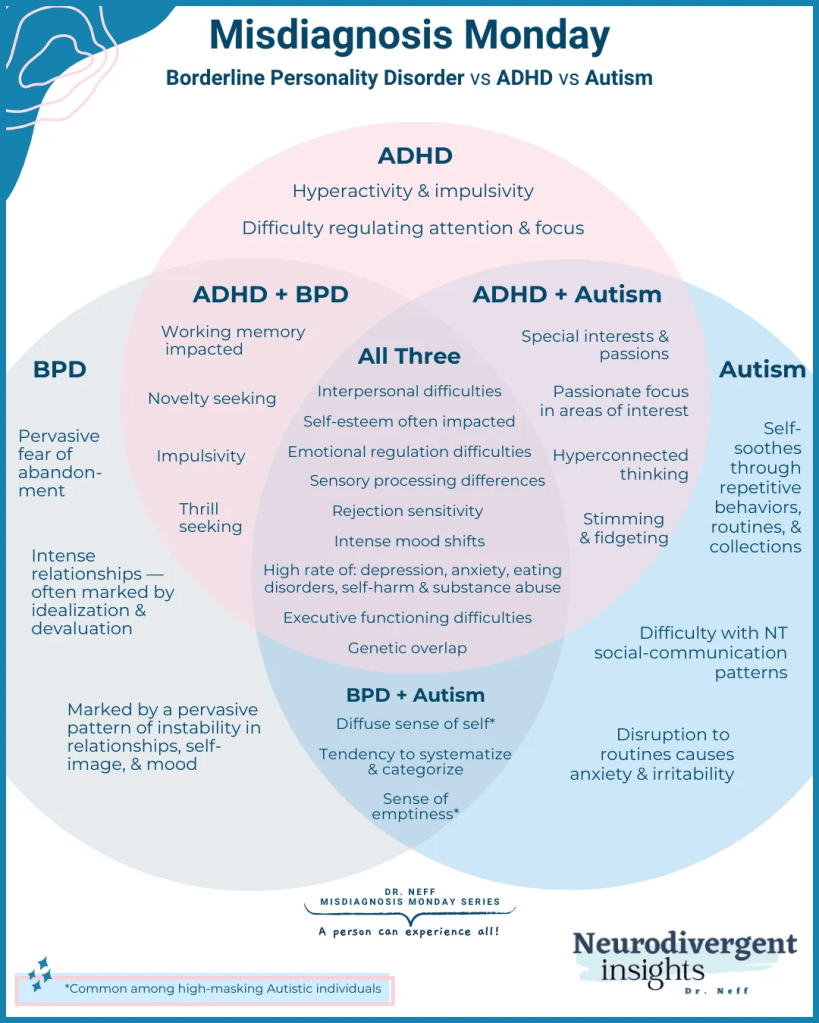
It’s important to note that sensory processing challenges aren’t exclusive to autism or ADHD – they can affect anyone, including those with BPD and other mental health conditions. BPD can also co-occur with other conditions like Anxiety, Depression, ADHD, and Autism – among so many others. If you find yourself irritated by tags in clothing or distracted by tiny background noises when you’re already upset, you’re not alone. Small annoyances in the environment can amplify emotional distress. And when your senses are overwhelmed, it’s way harder to manage your feelings.
When the Environment Triggers an Emotional Meltdown
Perhaps you’ve experienced something like this: you’re already having a rough day, and then you walk into a crowded store. The fluorescent lights are jarring, music is blaring, people are bumping into you. Suddenly, it’s all too much. Monsters. Crouched in every corner. You might feel a rush of panic or anger and before you know it – you’re in an emotional meltdown. The meltdown could be an angry outburst, uncontrollable crying, or shutting down completely. These episodes often seem to come “out of nowhere” to outsiders, but inside, a storm has been building. And you may be cognizant of the amounting or not.
Sensory issues like discomfort with clothing, temperature, or background noise add layers of irritation to an already fragile mood. One mental health resource gives a great example: if you’re calm and rested, you might handle a busy mall for a while, but on a bad day (tired, stressed, upset) the bright lights and noise might overwhelm you immediately. In BPD, these environmental “last straws” can tip you from coping to crisis. And this might happen frequently, edging you into fight-or-flight mode way more often than most, particularly when there is no “real threat.”
During the build-up to a meltdown, you might notice signals: your body is tense, you feel trapped or on edge, and everything starts to feel like nails on a chalkboard. Everything. There’s often a mix of emotional pain (“I feel rejected/hurt”) and physical unease (headache, nausea, jitters, or just a sense that your skin is crawling). When it crescendos, the meltdown hits.
For many, the meltdown itself feels like a release. All that bottled-up pressure explodes outward. You might yell, sob, throw something, or even be drawn to more physically dangerous outlets in the moment. The explosion is intense, utilizing and depleting most of your energy sources; then, almost suddenly, the intensity crashes down. There may even be a strange calm after the storm. The brain has hit reset by expelling all that energy. Crying or screaming can actually activate the body’s soothing mechanisms, which is why a burst of tears might leave you feeling numb or oddly relieved afterward. Unfortunately, that relief might be followed by guilt, shame, or exhaustion – a sort of emotional hangover. But in the moment, the meltdown is your system’s way of trying to purge the overwhelm.
If this sounds familiar, it’s important to remember that you’re not alone in experiencing these episodes; your brain and body are reacting to the overload, like many others are. Understanding this connection – that sensory overwhelm feeds into emotional overwhelm – can be the first step to gaining a bit more control. It also can help your loved ones be more compassionate, realizing that you’re not choosing to blow up or shut down; often, it’s a last-resort reaction when you’re pushed past your limits.
Learning Your Triggers and Early Warning Signs
Everyone’s sensory triggers can be different. Some common ones that people with BPD and other sensory sensitivities report are:
• Loud, sudden, or repetitive noises: For example, a dog barking nonstop or a blaring TV in the next room might make you increasingly tense without you even realizing it. Over time, it can push you toward an outburst.
• Crowded or chaotic environments: Busy restaurants, parties, shopping centers – the mix of voices, lights, and social expectations can drain your emotional battery fast.
• Physical discomfort or pain: Minor pain or discomfort can be amplified. Think of things like an itch you can’t scratch, being too hot or cold, hunger, or even a mild headache. These physical stressors often make emotional regulation much harder (ever notice how you might be more irritable when you’re hungry or tired?).
• Touch and personal space: Some individuals with BPD report being sensitive to touch – for instance, not liking to be hugged or touched unexpectedly when they’re upset. It’s not that they don’t crave comfort (often they do), but in a highly agitated state, even gentle touch can feel startling or intrusive. This heightened sensitivity to touch is documented in BPD – intense emotions can extend to intense physical sensations.
• Sensory “pet peeves”: Everyone has certain sensations that just set them off. Maybe the tag in your shirt drives you nuts, or the flicker of a fluorescent bulb gives you anxiety, or the smell of strong perfume makes you nauseous. When you’re emotionally raw, these minor sensory issues can become major aggravations.
Pay attention to your own patterns. You might even keep a journal noting when you had an episode and what was happening around you. Emotional meltdowns almost always have precursors: that pounding music next door put you on edge, or the clutter in your room made you feel out of control, before the real explosion. By identifying these, you can start addressing the triggers earlier – ideally before meltdown mode.
For example, if you notice you’re clenching your jaw and your heart’s racing because the side-chatter is too distracting while you’re working, that’s a sign to step away or put on headphones (more on coping tools soon). If a conversation is getting heated and you also feel uncomfortably cold and jittery, maybe pause to grab a sweater or a hot drink while you collect yourself. Tuning in to those early warning signs – both emotional and physical – is key. It’s a skill to build over time, but it can make a big difference in heading off full-blown crises.
The Meltdown Experience: Why It Feels Like a “Release”
We touched on this earlier, but let’s explore why a meltdown can actually feel relieving. Imagine your emotions and sensory inputs like a bottle of soda that’s been shaken up. The pressure is building and building inside. Keeping it all in (with the cap on tight) is agonizing – you feel that internal pressure as unbearable anxiety, anger, and physical tension. When a meltdown happens, it’s like the cap blew off the bottle. All that pent-up pressure bursts out.
Release.
In physiological terms, an intense emotional outburst can activate your parasympathetic nervous system after the peak of the storm. This is the part of your nervous system that says “Okay, danger passed – time to calm down now.” It’s the same system that kicks in after you have a good cry or after you narrowly avoid a car accident and pull over shaking – it helps slow your heart rate and breathing. That’s why sometimes after screaming or sobbing, you might suddenly feel tired or surprisingly calm. Your body’s relief response has taken over, at least temporarily.
Emotionally, a meltdown can also push the “reset” button on an overwhelming situation. In the moment, you might feel totally out of control – like the world is ending – but once it’s over, your brain sometimes goes, “whew, I let it out.” The problems aren’t gone, but that acute, unbearable peak of emotion has passed. One person likened their post-meltdown state to “suddenly my mood shifts back, and it’s as if nothing ever happened”. It’s not that nothing happened (and certainly the consequences of our meltdowns do happen), but internally there’s a drastic shift from 100% intensity back to baseline. That contrast can feel like relief.
However, this “relief” comes at a cost. Meltdowns can be traumatic for you and those around you. Often, after that calm, real life floods back in – you might see a loved one looking scared or hurt by your actions, or notice the mess you made, or recall things you shouted. Then feelings of guilt, shame, or sadness might hit hard. It’s common for people with BPD to feel deep remorse after an episode, which can loop back into the cycle of emotional pain.
That said, understanding that a meltdown was your body’s way of coping with overload (however destructive it may have been) can allow you to forgive yourself and start learning from it rather than just hating yourself for it. It’s like seeing that “shaken soda bottle” and thinking, okay, how can I avoid getting that shaken up in the first place? And if it does get shaken, how can I release a bit of pressure safely, so I don’t fully explode?
This is where coping skills and sensory tools come in. By managing your sensory and emotional overload on a day-to-day basis, you can prevent that pressure from reaching explosion point – or at least raise the threshold so it takes more to get you there.
Let’s look at some strategies that can help.
Sensory Tools and Coping Techniques for Emotional Regulation
Managing BPD often means tackling it from both angles: the emotional side and the physical/sensory side. It can be incredibly empowering to have a toolkit of strategies that soothe your senses and body, which in turn can calm your emotions. Below are some sensory tools and coping techniques that many people find helpful when dealing with sensory overwhelm and intense feelings.
• Creating a calming sensory space – like using a weighted blanket for comfort – can help signal your body to relax. Using supportive sensory tools can help you dial down the overload before it triggers a meltdown. Everyone is different, so you might need to experiment to find what works best for you. Here are a few ideas to consider (you can mix and match them, too!):
• Weighted Blankets: These are heavy blankets (filled with beads or pellets) that apply gentle pressure across your body, sort of like a firm hug. That steady pressure, known as deep pressure stimulation, can have a calming effect on the nervous system. Studies have suggested that weighted blankets may help reduce anxiety and improve sleep quality. Many people with anxiety or sensory issues report feeling safer and more grounded under a weighted blanket – it can ease that restless, skin-crawling sensation and help you feel centered.
• Noise-Canceling Headphones or Earplugs: If sounds are a trigger for you, investing in good noise-canceling headphones can be life-changing. They can muffle the external chaos and give you a pocket of quiet when you start feeling overwhelmed in loud environments. You can play calming music or just enjoy the silence. Many people with sensory sensitivity carry earplugs or headphones everywhere – and that’s a perfectly valid coping strategy, not something to be embarrassed about. Next time you’re heading into a potentially loud or busy place (like a grocery store, public transit, a family gathering), consider bringing these along. It can mean the difference between “okay” and “too much” for your nerves.
• Grounding Exercises: Grounding techniques help pull you out of the spiral of thoughts or the wave of sensory overload and bring you back to the present moment. Often, they involve engaging your five senses intentionally to counteract the panicky, lost-in-thought feeling. For instance, one popular exercise is the “5-4-3-2-1” method: look around and name 5 things you can see, 4 things you can physically feel (your feet on the floor, the texture of your shirt), 3 things you can hear right now, 2 things you can smell, and 1 thing you can taste (even if it’s just the lingering mint from toothpaste). By the time you go through these, your breathing may have slowed, and your mind is more in the here and now rather than racing with emotion.
Other sensory grounding tricks include holding an object (preferably with an interesting texture or meaning) and focusing on how it feels in your hand or listening intently to the sounds around you (like the hum of a fan), or smelling something soothing like a favorite essential oil or a scented candle. Some people take a warm bath or shower as a full-body grounding technique – the warm water can be very regulating. The key is to engage your senses in a neutral or positive way to balance out the negative overwhelm.
• Aromatherapy and Calming Scents: Our sense of smell is directly linked to the emotional center of the brain. Ever catch a whiff of a certain perfume or the smell of rain and instantly feel a certain way? You can use that to your advantage. Aromatherapy – using essential oils or scented products – is a simple tool to create a calming environment. Scents like lavender, chamomile, or vanilla are commonly found to be soothing. You might try an essential oil diffuser, or a pillow spray, or even just an inexpensive lavender-scented lotion that you can rub on your hands when you’re anxious (bonus: the act of massaging your hands with lotion can be another grounding activity). Citrus scents like orange or bergamot can be uplifting if you’re feeling low. Find a smell that makes you feel comforted or happy and keep it on hand.
• Creating a Sensory Safe Space: If possible, designate an area (a room, or even just a corner of a room) that you can retreat to when you’re overwhelmed. This space should be tailored to what soothes you. Maybe it’s dim lighting or a favorite lamp, comfy pillows or a weighted blanket, soft background sounds (white noise or nature sounds), and minimal clutter. Think of it as your recharge station. When you feel an episode brewing or you come home drained from sensory chaos outside, give yourself permission to spend time in this calming space. Even at work or on the go, identify little ways to create a safe bubble – carry sunglasses to dim bright lights, keep soothing music on your phone, have a comforting item in your bag (like a stress ball or a smooth stone). These small things can help ground you when the world feels hectic.
• Mindfulness and Breathing Exercises: These often go hand in hand with grounding. Mindfulness is basically practicing being present and aware without judgment. When everything is overwhelming, pausing to take a few slow, deep breaths is a mini-act of mindfulness that sends signals to your brain that you’re safe. There are lots of breathing techniques (4-7-8 breathing, box breathing, etc.), but even the simple act of consciously inhaling for a count of 4, exhaling for a count of 6 and repeating that can activate your parasympathetic “calming” system. Some people find guided meditation apps or relaxing music helpful – others prefer to just sit quietly and focus on one sensation (like the feel of their breath at the nostrils). The goal isn’t to magically erase your feelings, but to prevent that runaway train effect where one stressful thing leads to another until you derail. Mindfulness helps you catch the stress early and sit with it, so it doesn’t pile up into a meltdown. And remember, mindfulness is a skill – it gets easier with practice, so don’t worry if at first you feel too restless to sit still. Even one minute of deep breathing is better than none.
These are just a few tools – there are many others (exercise, journaling, art, talking to a supportive friend, therapy skills like DBT TIP skills, etc.) that can also help regulate intense emotions. But the ones above specifically target the sensory component of dysregulation. By calming your body and environment, you make it a lot easier to calm your mind.
Supporting Someone with BPD Through Sensory Overwhelm
If you’re reading this as someone who cares about a person with BPD, thank you for wanting to understand. Sensory overwhelm and emotional meltdowns can be baffling from the outside. One minute you’re chatting, the next your loved one is snapping or in tears over something that seemed minor. It’s easy to misinterpret these reactions as drama, attention-seeking, or “craziness,” but as we’ve discussed, there is always more under the surface. Sensory and emotional discomfort build up to a breaking point.
Here are a few tips for supporters:
• Validate and remain calm: During a meltdown (or when you see one coming), try not to say things like “you’re overreacting” or “calm down.” Instead, a gentle “I’m here, I know it’s a lot right now” goes a long way. Keep your voice steady and low, because raising your voice or showing panic can add to their overload.
• Reduce stimuli: If possible, help adjust the environment. Turn off bright lights, switch off any loud TV or music, ask others in the area to give some space. Offer something comforting like a glass of water, a cool washcloth, or a quiet room. You can even suggest a coping tool: “Would it help if we step outside for some air?” or “Do you want your headphones?” They may say no, but just asking shows you get it.
• Don’t take it personally: BPD meltdowns can include angry words – remember that this is the person’s pain and overwhelm speaking. It’s not a deliberate attack on you. Give them space if they indicate they need it (“I’ll be right in the next room if you need me” can reassure them you’re not abandoning them while respecting their space). Many individuals with BPD can feel easily smothered, despite their yearning for closeness.
• Aftercare: Once the storm passes, your loved one might feel embarrassed or guilty. Gently reassure them. You might say, “I know that was really hard for you. It’s okay, I’m not angry at you. Do you need a hug or anything right now?” They might want to talk about what triggered it or they might not – let them lead. Later on, during a calm moment, you could bring up, “I read that certain things like noise or stress can build up for you. Is there anything I can do in the future when I notice you’re getting overwhelmed?” This way you team up with them against the problem (the overload), rather than seeing them as the problem.
Supporting someone through this requires patience and empathy, but it can greatly improve trust and reduce the intensity of episodes over time. Just knowing that someone is trying to understand what you’re going through is incredibly healing for a person with BPD. Demystifying the condition by not fixating too much on “the diagnosis” can also reduce shame, guilt, and avoidance for the individual.
Moving Forward with Compassion and Hope
Living with BPD and sensory processing challenges is not easy, but it’s important to remember that having a sensitive system also means you perceive a lot of the beauty and detail others might miss. You may feel emotions (and even sensations) more vividly – which can be a strength in the right circumstances. Still, you’ll need to take care of yourself a bit differently, with awareness of your triggers and proactive soothing strategies. And that’s okay. In fact, it’s extremely resourceful to identify what helps you and to use it.
Over time, you might find that with therapy (like Dialectical Behavior Therapy, which is often recommended for BPD, in conjunction with a sensory processing approach) that your meltdowns become less frequent or less intense. You’ll start catching the warning signs earlier and feel more in control. It’s a journey – there will still be bad days, and that’s alright. What matters is that you’re trying and learning.
Remember to celebrate the little victories: the day you left the party before you started screaming, because you noticed you were getting overwhelmed and took a breather outside instead. Or the time you felt the urge to self-harm rise up, but you grabbed your weighted blanket and put on calming music, and the urge passed. Those moments are HUGE, even if no one else sees them.
It’s easy to feel like you’re “too sensitive” or “burdening others” and thus ignore your own needs. But everyone has the right to live in an environment that feels safe and supportive. Take it one day at a time, one sensation at a time. With understanding, the right tools, and a lot of compassion (for yourself above all!), it’s absolutely possible to navigate a world that feels “too much” and find your balance. You’ve got this.
References
1. Sensory Overload in Adults – It’s Not Just an Autism Thing – Harley Therapy™ Blog
2. Borderline Personality Disorder, ADHD, and Autism – Neurodivergent Insights
3. Coping Skills for Borderline Personality Disorder

Leave a reply to Coping Techniques for Sensory Sensitivity in BPD – Living Level Cancel reply